Pancreatitis and Diabetes: Understanding the Connection
How Are Pancreatitis and Diabetes Connected?
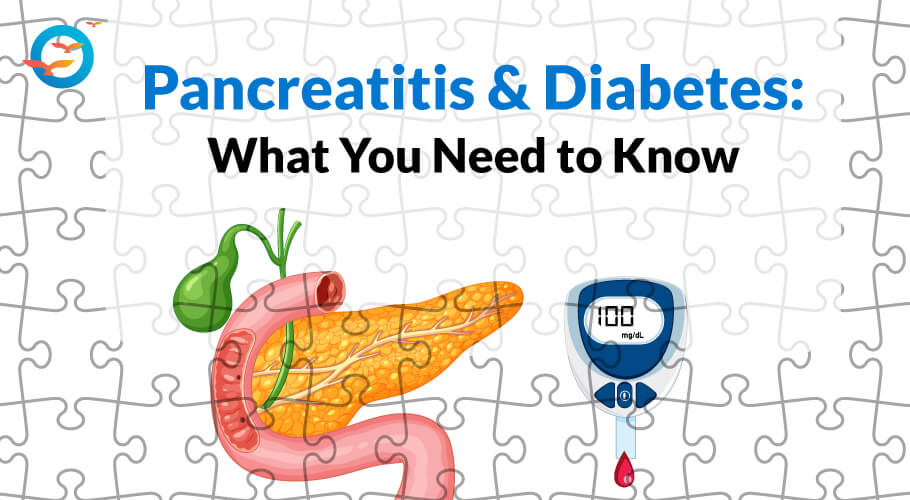
Pancreatitis and diabetes are two interconnected conditions that significantly impact overall health. Pancreatitis, the inflammation of the pancreas, disrupts its vital functions in digestion and blood sugar regulation.
Diabetes, a chronic condition characterized by high blood sugar levels, often arises from or worsens due to pancreatic dysfunction. Understanding the link between these conditions is crucial, as managing one can influence the course of the other.
In this blog, we will explore the relationship between pancreatitis and diabetes, discussing their causes, symptoms, treatments, and the importance of a comprehensive approach to care for individuals affected by both. Read the full blog and learn how to regenerate pancreas beta cells naturally.
What Is Pancreatitis?
Pancreatitis is an inflammation of the pancreas, a vital organ behind the stomach involved in digestion and blood sugar regulation. It occurs when digestive enzymes activate inside the pancreas, causing irritation and inflammation.
Pancreatitis can be acute (sudden and short-term) or chronic (long-lasting), with common causes including gallstones, excessive alcohol consumption, certain medications, and genetic factors.
What Are the Symptoms of Pancreatitis?
Symptoms include severe abdominal pain, nausea, vomiting, and fever. In severe cases, it can lead to complications like infection, bleeding, and damage to other organs.
Pancreatitis and Diabetes: The Interconnection
Pancreatitis and diabetes are not mutually exclusive; in fact, they can influence each other significantly. Pancreatitis can impair the pancreas's ability to produce insulin, leading to or exacerbating diabetes. Conversely, individuals with diabetes, particularly type 2, are at a higher risk of developing pancreatitis due to the strain diabetes places on the pancreas.
Chronic pancreatitis can cause long-term damage to pancreatic tissue, resulting in the loss of insulin-producing cells and consequently causing diabetes, often referred to as pancreatogenic or type 3c diabetes. Therefore, the relationship between these conditions is interdependent, and managing one can affect the other.
Diet Tips for Pancreatitis & Diabetes
Managing pancreatitis with diabetes requires special dietary care to ensure both conditions are effectively controlled.
- Foods that can be included are lean meats, plenty of fruits, vegetables, whole grains, and low-fat dairy products.
- Healthy fats, such as those from nuts, seeds, and avocados, are also beneficial but should be consumed in moderation.
- It's crucial to avoid high-fat foods, fried foods, sugary snacks, and beverages, as these can exacerbate pancreatitis and destabilize blood sugar levels.
- We can also include coconut oil and amla.
- Usage of calming tea like chamomile and mint tea can also be helpful in this condition.
- Alcohol should be completely avoided due to its detrimental effects on both the pancreas and blood sugar regulation.
- A well-balanced diet focusing on nutrient-rich, low-fat, and low-sugar foods is key to managing these conditions simultaneously.
Lifestyle changes
- To avoid and treat pancreatitis, adopting certain lifestyle choices is essential.
- Maintaining a healthy diet low in fat and sugar, and rich in fruits, vegetables, lean proteins, and whole grains can significantly reduce the risk.
- Avoiding excessive alcohol consumption and quitting smoking are critical, as both are major risk factors for pancreatitis.
- Regular physical activity helps maintain a healthy weight and supports overall pancreatic health.
- Managing stress through relaxation techniques such as yoga or meditation can also be beneficial.
- For those with a history of pancreatitis, adhering strictly to medical advice, including prescribed medications and follow-up care, is vital for preventing recurrences and promoting recovery.
Conclusion
In conclusion, pancreatitis and diabetes are complex, interrelated conditions that require careful management and lifestyle adjustments. Understanding the connection between the two can help in the early detection and treatment of both diseases. Implementing a balanced diet, avoiding alcohol and smoking, maintaining a healthy weight, and adhering to medical advice are crucial steps in managing these conditions. In this blog you learnt how to regenerate pancreas beta cells naturally.
By taking proactive measures and seeking appropriate medical care, individuals can improve their quality of life and reduce the risk of complications associated with pancreatitis and diabetes. Remember, ongoing support from healthcare providers, family, and the community plays a vital role in effectively managing these health challenges.
Learn more about how fatty liver can influence diabetes management. Visit our detailed article on Fatty Liver and Diabetes.
FFD's contribution:
At FFD, we implement a comprehensive plan for participants based on four key protocols: diet, exercise, inner transformation, and medical care. This approach has successfully reversed diabetes for many and enhanced pancreatic health.
Take care of your health!
FAQ
What is the connection between pancreatitis and diabetes?
Pancreatitis can damage the pancreas, making it harder for the body to produce insulin. This can lead to diabetes.
Can pancreatitis cause diabetes?
Yes, Chronic pancreatitis can damage the pancreas, leading to loss of insulin-producing cells and causing the diabetes.
What are the symptoms of pancreatitis that might indicate a risk of diabetes?
Symptoms include Severe abdominal pain, Nausea, vomiting, and fever. In severe cases, it can lead to complications like infection, bleeding, and damage to other organs.
How can diabetes be managed if you have pancreatitis?
Managing diabetes with pancreatitis involves monitoring blood sugar levels closely. Implementing a balanced diet, avoiding alcohol and smoking, maintaining a healthy weight, and adhering to medical advice.
Can treating pancreatitis help control diabetes?
By taking proactive measures and seeking appropriate medical care, individuals can improve their quality of life and reduce the risk of complications associated with pancreatitis and diabetes.
What lifestyle changes can help manage both pancreatitis and diabetes?
Balanced diet, Avoiding alcohol, Regular exercise, and maintaining a healthy weight are crucial for managing both conditions.
Are there specific diets recommended for people with both pancreatitis and diabetes?
A well-balanced diet focusing on nutrient-rich, low-fat, and low-sugar foods is key to managing these conditions simultaneously.