Diabetic Foot Ulcer: Causes and Treatments
Diabetes, if unattended, can lead to a range of serious complications affecting various parts of the body. When blood sugar is not controlled it damages blood veins resulting in complications like nephropathy, neuropathy and so on. Today, we are going to focus on the topic of diabetic foot ulcer. For that we need to understand neuropathy first.
What is Neuropathy?
Neuropathy, a prevalent complication of diabetes, often leads to foot injuries due to nerve damage caused by prolonged high blood sugar levels. This nerve damage, particularly in peripheral neuropathy, diminishes sensation in the feet, making it difficult for individuals to feel pain, temperature changes, or injuries. As a result, minor cuts, blisters, or sores can go unnoticed and untreated, potentially developing into severe infections or ulcers.
What is Diabetic Foot Ulcer?
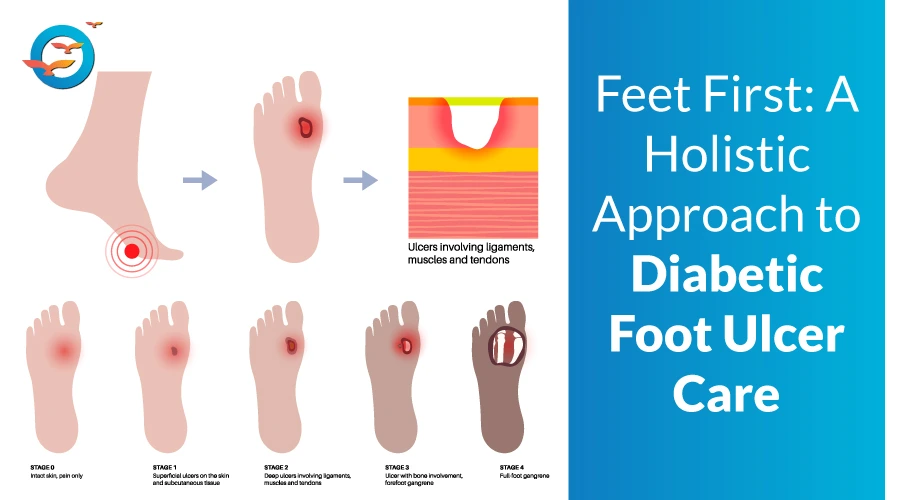
Diabetic foot ulcers are one of the most severe complications associated with diabetes. These ulcers can significantly impact the quality of life and, if left untreated, can lead to severe infections, amputations, and even death. Understanding the causes and treatments of diabetic foot ulcers is crucial for effective management and prevention.
Diabetic Foot Ulcer Causes
1. High Blood Sugar Levels:
Persistent high blood sugar levels can damage nerves and blood vessels, leading to reduced sensation (neuropathy) and poor circulation. This makes it difficult for injuries to heal and increases the risk of infection.
2. Peripheral Neuropathy:
Nerve damage from diabetes can cause loss of sensation in the feet. This means minor cuts, blisters, or pressure sores may go unnoticed and untreated, leading to ulcers.
3. Poor Circulation:
Diabetes can lead to peripheral arterial disease (PAD), where blood vessels narrow, reducing blood flow to the extremities. Poor circulation impairs wound healing, making ulcers more likely.
4. Foot Deformities:
Conditions such as hammertoes, bunions, or Charcot foot, common in people with diabetes, can create pressure points that lead to skin breakdown and ulcers.
5. Inadequate Foot Care:
Poor foot hygiene, wearing ill-fitting shoes, and neglecting regular foot inspections can contribute to the development of ulcers.
What is the treatment for Diabetic Foot Ulcers?
Diabetic foot ulcer can be treated as follows-
1. Blood Sugar Control:
Maintaining optimal blood glucose levels is critical. This helps prevent further nerve and blood vessel damage and promotes healing.
2. Wound Care:
Proper wound care is essential for treating diabetic foot ulcers. This includes cleaning the wound, removing dead tissue (debridement), and applying dressings to keep the ulcer moist and protected.
3. Antibiotics:
If an infection is present, antibiotics may be prescribed to treat it. It's crucial to follow the prescribed course to prevent the infection from worsening.
4. Offloading:
Reducing pressure on the ulcerated area is vital. This can be achieved using special shoes, casts, or braces designed to relieve pressure and protect the foot.
5. Surgical Intervention:
In severe cases, surgical procedures may be necessary to remove infected tissue, correct deformities, or improve blood flow to the affected area.
6. Hyperbaric Oxygen Therapy (HBOT):
HBOT involves breathing pure oxygen in a pressurized room. This therapy can enhance wound healing by increasing oxygen supply to the affected tissues.
7. Patient Education:
Educating patients on proper foot care, including daily inspections, moisturizing, wearing appropriate footwear, and avoiding walking barefoot, is crucial for preventing ulcers.
How to prevent Diabetic Foot Ulcers?
1. Regular Check-Ups:
Regular visits to a healthcare professional for foot examinations can help detect and address potential issues early.
2. Proper Footwear:
Wearing shoes that fit well and provide adequate support can prevent pressure points and injuries.
3. Daily Foot Care:
Washing feet daily, keeping them dry, and inspecting them for any signs of injury or infection can help catch problems early.
4. Blood Sugar Management:
Consistently managing blood sugar levels through diet, exercise, and medication can prevent complications that lead to foot ulcers.
Conclusion
Diabetic foot ulcers are a serious complication that requires prompt attention and proper management. Understanding the causes and available treatments can help individuals with diabetes take proactive steps to prevent and treat foot ulcers, ultimately improving their quality of life and reducing the risk of severe outcomes. By maintaining good foot hygiene, managing blood sugar levels, and seeking regular medical care, individuals can significantly reduce the risk of developing diabetic foot ulcers.
Role of FFD in helping stay away from diabetic complications-
At Freedom from Diabetes, we assist individuals in reversing their diabetes and its related complications. Our successful diabetes reversal cases are continually increasing. You can join our Discover Reversal Session to learn about the process of reversing diabetes. Become a part of our annual Holistic Transformation program, and rest assured that you'll be taking steps to avoid diabetic complications such as foot ulcers.
FAQs
What is neuropathy and how does it affect my feet?
Neuropathy is nerve damage caused by high blood sugar levels. It reduces sensation in my feet, making it hard to notice injuries, which can lead to ulcers and infections.
How do I know if I have a diabetic foot ulcer?
I should look for signs like redness, swelling, drainage, or an open sore on my foot. If I notice any of these, I should consult a doctor immediately.
Can a diabetic foot ulcer heal on its own?
No, without proper care, it can worsen. I need to keep my blood sugar controlled, clean the wound, and follow my doctor’s advice for faster healing.
What should I do if I have a foot ulcer?
I should clean the wound, avoid putting pressure on it, wear protective footwear, and seek medical attention immediately to prevent complications.
How can I prevent diabetic foot ulcers?
I should check my feet daily, wear proper shoes, control my blood sugar, and keep my feet clean and moisturized.
Is walking safe if I have a foot ulcer?
Walking can put pressure on my ulcer, slowing healing. I should use offloading techniques like special footwear or braces to reduce pressure.